The Gut-Brain Axis: A Vital Link Between Gut Microbiota and Mental Health
A Scientific Looks into How Your Gut Microbiome Affects Mental Wellness.
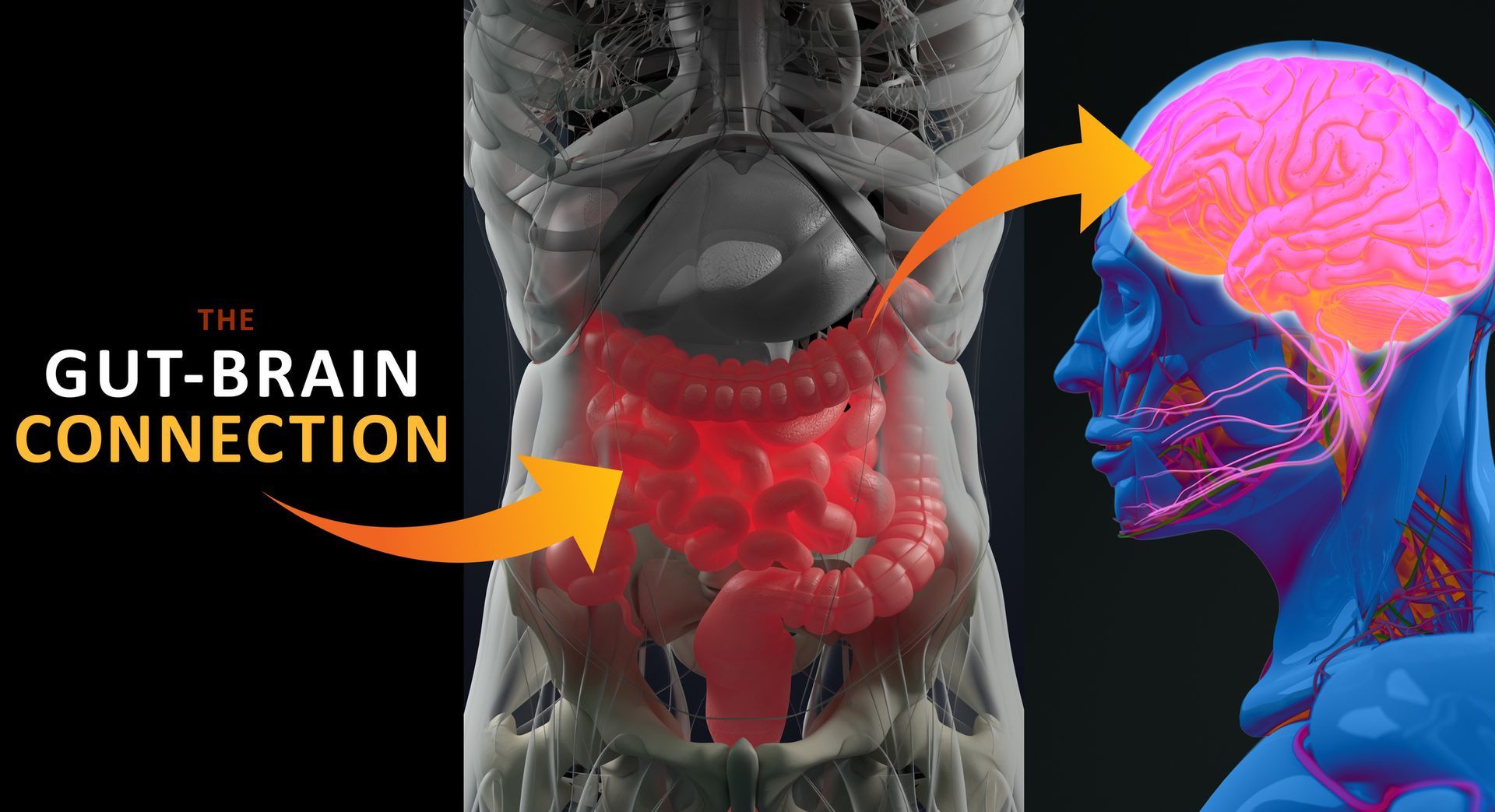
The gut-brain axis represents a complex, bidirectional communication system that connects the central nervous system (CNS) with the enteric nervous system (ENS) located in the gastrointestinal tract. This intricate network involves a multitude of signaling mechanisms, including neural, hormonal, and immunological pathways. Central to this communication is the vagus nerve, a key cranial nerve that facilitates neural exchanges between the gut and the brain. Additionally, the gut microbiota plays a crucial role by producing bioactive compounds—such as short-chain fatty acids (SCFAs), neurotransmitters, and various metabolites—that can significantly influence brain function and mental health.
The Role of Microbiota in Neurotransmitter Production
One of the most impressive ways in which gut microbiota affects mental health is through its ability to produce essential neurotransmitters. Notably:
- Serotonin: Often referred to as the "feel-good" neurotransmitter, serotonin is vital for regulating mood, sleep, and appetite. Remarkably, around 90% of the body's serotonin is synthesized in the gut, where specific microbes facilitate its production.
- GABA (Gamma-Aminobutyric Acid): This neurotransmitter is crucial for reducing anxiety and fostering relaxation. Certain gut bacteria, particularly species from the Lactobacillus and Bifidobacterium genera, are known to produce GABA.
- Dopamine: Associated with motivation and pleasure, dopamine production is also influenced by the gut microbiota.
The ability of gut microbiota to impact the levels of these neurotransmitters highlights its significant potential to affect mood and behavior.
Gut Microbiota’s Influence on Stress Response
The gut microbiome plays a key role in modulating the body's response to stress. Chronic stress can disturb the balance of microorganisms in the gut, leading to a condition known as dysbiosis. This imbalance can exacerbate stress by promoting inflammation and altering hormone levels. Notably, cortisol, the primary stress hormone, is closely linked to gut health. Research indicates that a healthy gut microbiome can help regulate the hypothalamic-pituitary-adrenal (HPA) axis, which is responsible for managing the body's stress responses.
Mental Health Disorders and Gut Microbiota
The relationship between gut health and mental health is becoming increasingly clear across various psychological conditions, including:
- Depression: Research has indicated that individuals suffering from depression frequently display altered gut microbial diversity, often characterized by a reduction in beneficial bacteria such as Bifidobacterium and Lactobacillus.
- Anxiety Disorders: Dysbiosis in the gut has been associated with heightened anxiety-like behaviors. Animal studies have shown that introducing healthy gut microbiota can alleviate anxiety symptoms.
- Autism Spectrum Disorders (ASD): Emerging studies suggest that children with ASD display distinct gut microbiota profiles, potentially contributing to their behavioral symptoms. Targeted interventions aimed at improving gut health are being investigated as potential therapies.
- Cognitive Decline and Neurodegenerative Diseases: Conditions like Alzheimer’s and Parkinson’s disease have been linked to imbalances in gut microbiota. Research suggests that inflammation within the gut may accelerate neurodegenerative processes.
Innovations and Research Advances
The rapid expansion of microbiome research has led to exciting discoveries and innovative therapeutic approaches, including:
- Psychobiotics: These are probiotics designed specifically to target mental health issues. They can modulate the gut-brain axis and potentially alleviate symptoms of depression, anxiety, and stress.
- Fecal Microbiota Transplantation (FMT): Originally developed for treating recurrent Clostridioides difficile infections, FMT is now being investigated for its potential to restore microbial balance in individuals with mental health disorders.
- Microbial Metabolites: Researchers are identifying specific metabolites produced by gut bacteria—like SCFAs and tryptophan metabolites—that may serve as new therapeutic targets for brain health.
- Dietary Interventions and Nutrition: Diet significantly influences gut microbiota. High-fiber, plant-based diets rich in prebiotics can support healthy bacteria and potentially enhance mental well-being.
Challenges in Gut Microbiota Research
Despite its promising potential, research into gut microbiota faces several challenges. The high variability in microbial composition among individuals complicates the identification of universal therapeutic targets. Additionally, distinguishing between correlation and causation in the links between microbiota and mental health remains a complex issue. Ethical considerations surrounding interventions like FMT and the use of genetically engineered microbes also require careful scrutiny.
Ethical and Social Considerations
As microbiota-based therapies gain traction, it’s essential to address their ethical and social implications. Ensuring equitable access to these treatments, protecting patient data privacy, and promoting public understanding of microbiome science are critical priorities. Public education can help dispel myths and foster informed decision-making regarding gut health and its impact on mental well-being.
Future Directions in Gut Microbiota Research
The future of gut microbiota research in relation to mental health is promising, with several key areas of exploration:
- Personalized Medicine: Advances in microbiome profiling may allow for tailored treatments based on an individual's unique microbial composition.
- Synthetic Biology: Engineering microbes to produce specific neurotransmitters or therapeutic compounds could transform mental health care.
- Longitudinal Studies: Monitoring changes in the microbiome over time can provide deeper insights into its role in mental health across different life stages.
- Integration with AI: The application of machine learning and AI to analyze complex microbiome data may reveal patterns and potential interventions.
Conclusion
The profound influence of gut microbiota on mental health marks a significant shift in our understanding of psychology and neuroscience. From modulating neurotransmitter production to shaping stress responses and influencing psychological disorders, the gut-brain connection presents a novel perspective on treating mental health conditions. As ongoing research continues to unveil the complexities of this relationship, microbiota-based therapies hold the potential to revolutionize mental health care. By adopting a multidisciplinary and ethical approach, we can open new doors to enhancing mental well-being and overall health.